Vast Differences in Legionnaires’ Disease Response by Industry
Outside of healthcare, few rules for preventing spread of the deadly bacteria in buildings.

The Western North Carolina Agricultural Center, shown here in October 2014, was the site of a Legionnaires’ disease outbreak in September 2019 that sickened 142 people. Photo courtesy of Performance Impressions LLC
By Brett Walton, Circle of Blue
Before a deadly outbreak of Legionnaires’ disease at an agricultural fair in western North Carolina last month, no one in the area had any idea of the damage to come.
Fairgoers and state health officials alike were oblivious to the health risk that lurked in the plumbing of the Davis Event Center, the structure at the heart of the outbreak, because the building’s water had never been tested for Legionella. Andrea Ashby, a North Carolina Department of Agriculture and Consumer Services spokesperson, confirmed this fact to Circle of Blue.
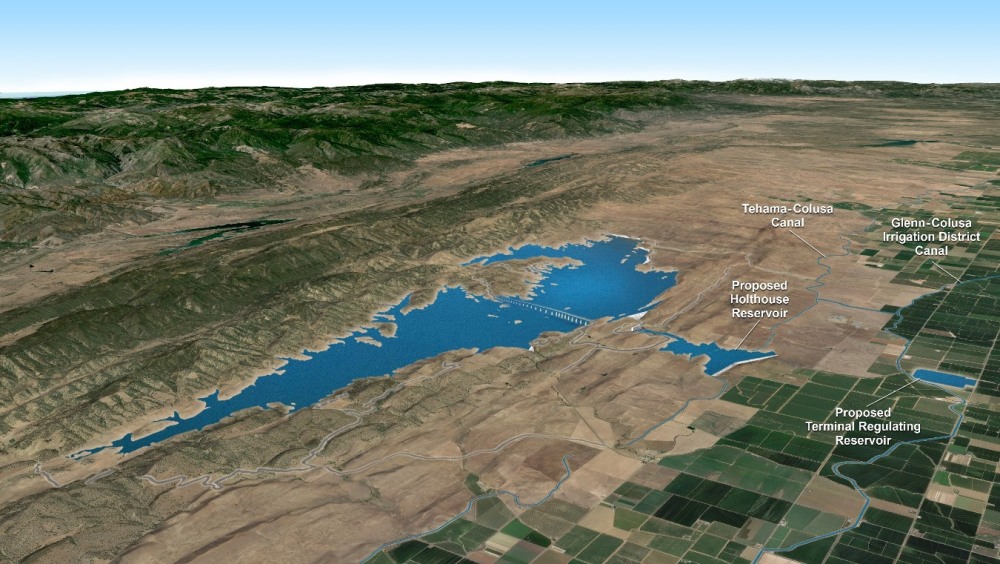
Once they noticed the disease cluster in late September, North Carolina health officials began an investigation that started to fill some of the information gaps. State health officials linked the outbreak, which has sickened 142 people and killed four, to hot tubs on temporary display at the Davis Event Center, an exhibition hall at the Western North Carolina Agricultural Center, near Asheville.
Legionnaires’ disease, which resembles pneumonia, and Pontiac fever, a less virulent illness similar to the flu, are contracted by inhaling water droplets contaminated with Legionella bacteria. North Carolina health officials believe that people attending the Mountain State Fair, which was held at the agricultural center between September 6 and 15, were exposed when they walked by the hot tubs, which generate steam that can be inhaled.
The hot tubs were a transmission site, but state health officials also found the bacteria within the Davis Event Center’s plumbing system. Water samples taken from a women’s bathroom faucet during the investigation tested positive for Legionella, though it was a genetically different strain than that isolated from people sickened during the outbreak.
The lack of water testing before the outbreak is not unusual. There are few regulations in the United States for monitoring building plumbing for Legionella. The rules that do exist largely target the healthcare industry.
Outside of healthcare, building owners generally are doing very little to prevent bacterial growth in their plumbing, according to interviews with people involved in Legionella testing and monitoring. Standards and industry best practices are followed haphazardly.
“With respect to other industries, sadly we typically only get involved when there’s an issue,” Russell Nassof, founder of the health risk consulting firm RiskNomics, told Circle of Blue. “Very rarely do we get companies that are being very proactive.”
Hotels and the hospitality industry are a high-risk sector. They operate large buildings with complex plumbing and may use decorative fountains, hot tubs, or other warm-water features that are known to incubate and spread the bacteria. In July, for instance, there were 14 confirmed cases of Legionnaires’ disease and 67 probable cases associated with a cooling tower at the Sheraton Atlanta Hotel. It was the largest Legionnaires’ outbreak in Georgia history.
As the founder of HC Info, which sells software for tracking building water management plans, Matt Freije sees repeated patterns of inaction among building owners. Only after an illness is identified do they react. He doesn’t foresee much change until owners are obliged to take precautionary measures.
“The writing is clearly on the wall,” Freije told Circle of Blue. “Most of them are not going to do anything they don’t have to do.”
Grant Newhouse, the CEO of Sustainable Water Solutions, a water treatment company, has observed gradual changes in the healthcare industry: the largest facilities were early adopters and medium-sized facilities had slower uptake, while smaller operations did not act “until they received a letter ordering it.”
“The rest of the industries are like that,” Newhouse told Circle of Blue. “The bigger facilities may be doing something, but there’s much less for smaller ones.”
Nassof, who lives in Las Vegas, said that the big casinos on The Strip are aware and actively addressing the risk. The Aria Resort and Casino, in the upmarket City Center development, had an outbreak in 2011 that attracted attention from major establishments, “but in general, your average, run-of-the-mill hotel is generally not interested unless they have an issue,” he said.
Why would a building owner not be more vigilant about their plumbing? Ignorance is gradually becoming less of a defense as more outbreaks occur, Nassof argued. But, especially for smaller operators, it also comes down to a lack of time, money, staff, and other resources, Freije said.
In 2015, ASHRAE, the group that represents the building systems industry, released a widely cited standard for managing building water systems to prevent Legionella growth. Freije, who has worked on Legionella prevention for 25 years, thought building owners would be more proactive following the publication of an accepted standard and its eventual endorsement by the Centers for Disease Control and Prevention. He found that his assumption was wrong.
“They haven’t,” he said.
Potential Rules Changes
The healthcare industry, which serves the people who are most vulnerable to Legionnaires’ disease, was the first to act in a comprehensive manner on Legionella prevention. But it did so only at the prompting of the federal government.
In June 2017, the Centers for Medicare and Medicaid Services, a division of the federal Department of Health and Human Services, started requiring hospitals and nursing homes that receive Medicare payments to have plans for maintaining building plumbing, testing water sources, and identifying areas at risk of Legionella growth. In 2014, the Veterans Health Administration issued a directive that required Legionella management plans and quarterly water testing at the more than 1,200 federal veterans’ healthcare facilities.
The bacteria are present in rivers and lakes, but they flourish in warm, stagnant water inside building plumbing and fixtures. The overall death rate for the disease, the deadliest waterborne illness in the country, is about one in 11, according to the Centers for Disease Control and Prevention. But for those who get sick in a healthcare setting, the rate is more like one in four. The number of reported cases is rapidly increasing, up five-fold since 2000.
A committee of Legionella experts recommended in a report released in August that all public buildings be required to have water management plans for preventing the growth of Legionella. Such rules exist in France, noted the committee, which was convened by the National Academies of Sciences, Engineering, and Medicine.
The Western North Carolina Agricultural Center falls into the public building category. It is owned by the state and operated by the North Carolina Department of Agriculture and Consumer Services.
The National Academies committee offered other actions for reducing the risk of bacteria transmission. The committee, for instance, recommended that state and local authorities maintain a registry of cooling towers.
A common breeding ground for the bacteria, cooling towers remove heat from building systems through evaporation. Because they disperse a fine mist into the air, they are frequently pinpointed as the source of Legionnaires’ outbreaks. An outbreak in the Bronx in July 2015 that sickened 138 people and killed 16 was traced to a hotel cooling tower.
After that incident, New York City health officials ordered building owners to register the location of all cooling towers, as well as maintain and inspect them.
Besides rooftop cooling towers, hotel plumbing systems have inherent risks. Legionella flourish in warm, stagnant water. Occupancy rates ebb and flow with the seasons, especially in tourist areas. When rooms are empty and showers and faucets are not being used, the bacteria have an opportunity to multiply.
Intermittent water use could be a factor at the Davis Event Center, where often several weeks passed between events. Ashby, the Department of Agriculture and Consumer Services spokesperson, was not able to say whether the plumbing at the center was ever flushed between events.
Because of the reactive nature of industries to Legionella, the North Carolina outbreak may resonate in a sector that previously had little frontpage exposure to the disease, Newhouse said.
“I don’t know how many purveyors of fairs knew to think about Legionella,” Newhouse said. “That list would be very, very short. But I think that next year many more will.”
Brett writes about agriculture, energy, infrastructure, and the politics and economics of water in the United States. He also writes the Federal Water Tap, Circle of Blue’s weekly digest of U.S. government water news. He is the winner of two Society of Environmental Journalists reporting awards, one of the top honors in American environmental journalism: first place for explanatory reporting for a series on septic system pollution in the United States(2016) and third place for beat reporting in a small market (2014). He received the Sierra Club’s Distinguished Service Award in 2018. Brett lives in Seattle, where he hikes the mountains and bakes pies. Contact Brett Walton









I didn’t know that cooling towers are a common breeding ground for bacteria. If I had one, I’d like it to be maintained properly. That way bacteria does not grow in it.